Geriatric Depression - Unheard of Yet Potentially Universal

By Patricia Zhang
Introduction to the Disease
Let's introduce three elderly figures whose physical and mental health are not as good as they could be: 76-year-old Mr Li, who suddenly felt weak and lost 40 pounds in just six months; 50-year-old Auntie Wang, who suffers from insomnia of such severity she has to take four sleeping pills every night before she can fall asleep; and 60-year-old Mr Zhang, who is often out of control and storms out of his mind over trivial matters. At first glance, there seems to be no resemblance between the conditions of these three elderly people, but in fact, all three suffer from depression - the main culprit that is "taking a toll" on their physical and mental health.
According to the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders - DSM-5, people who suffer from depression tend to be characterized by two things: they experience sadness, emptiness, or irritability, and along with that, there are cognitive changes that may occur and cause the experience of memory and concentration loss as well as slowed thinking. Gradually, the patient's overall ability to perform decreases, and the things they previously loved no longer interest them. Often they no longer want to participate in any events anymore, and that's how depression negatively affects people's daily behaviour.

Causation of disease
The causes of depression in older adults usually include the interplay of biology and the social environment.
On the biological side, genetic factors figure prominently, with research suggesting that a family history of depression as well as a genetic predisposition can increase the risk of developing depression, with heritability estimates ranging from 30% to 40%. In addition, imbalances in neurotransmitters, particularly deficiencies in serotonin and norepinephrine, have been linked to mood disorders and depression. Hormonal changes, such as menopause for women, are also thought to be one of the biological causes of depression, with about 10-15% of women experiencing symptoms of depression during menopause.
Sociocultural factors also play an important role: Social isolation is a common social factor, with about 43% of older adults feeling lonely regularly, and cultural stigma (older adults' fear of social ostracism for mental illness) may prevent up to 60% of older adults from actively seeking help. In addition, older adults face a 63% higher risk of stress and depression in their capacity as home caregivers for others.
Financial factors also play a significant role in social factors, with financial stress leading to approximately 20% of older adults living in poverty and experiencing depressive symptoms. Finally, bereavement is also an important social factor, with grief and the loss of a loved one potentially leading to a 30-40% increase in depression symptoms in older adults.

Measures of depression
1. a depressed state of mind almost every day and most of the day, either reported subjectively (e.g., feelings of sadness, emptiness, hopelessness) or observed by others (e.g., manifested by tearfulness). (Note: in children and adolescents, this may be manifested as irritability).
2. a marked decrease in interest or pleasure in all or almost all activities almost every day and for most of the day (either stated subjectively or observed).
3. significant weight loss without dieting, or weight gain (e.g., a change in weight of more than 5% of the original weight in one month), or loss or increase in appetite almost every day (note: children may exhibit failure to achieve standard weight).
4. insomnia or excessive sleepiness on an almost daily basis.
5. almost daily psychomotor agitation or retardation (fidgeting or slowness as seen by others, not just experienced subjectively).
6. fatigue or lack of energy almost every day.
7. almost daily feelings of worthlessness or excessive and inappropriate feelings of guilt (which can reach delusional proportions and are not merely self-condemnation or guilt due to illness).
8. almost daily presence of diminished thinking ability, inability to concentrate, or indecisiveness (can be either a subjective statement or an observation by others).
9. recurrent thoughts of wanting to die (rather than just fear of death), recurrent suicidal ideation without a specific plan, some kind of suicide attempt, or some specific plan to carry out the suicide.
When at least five of the above symptoms occur weekly, a diagnosis of depression is essentially confirmed.
Treatment
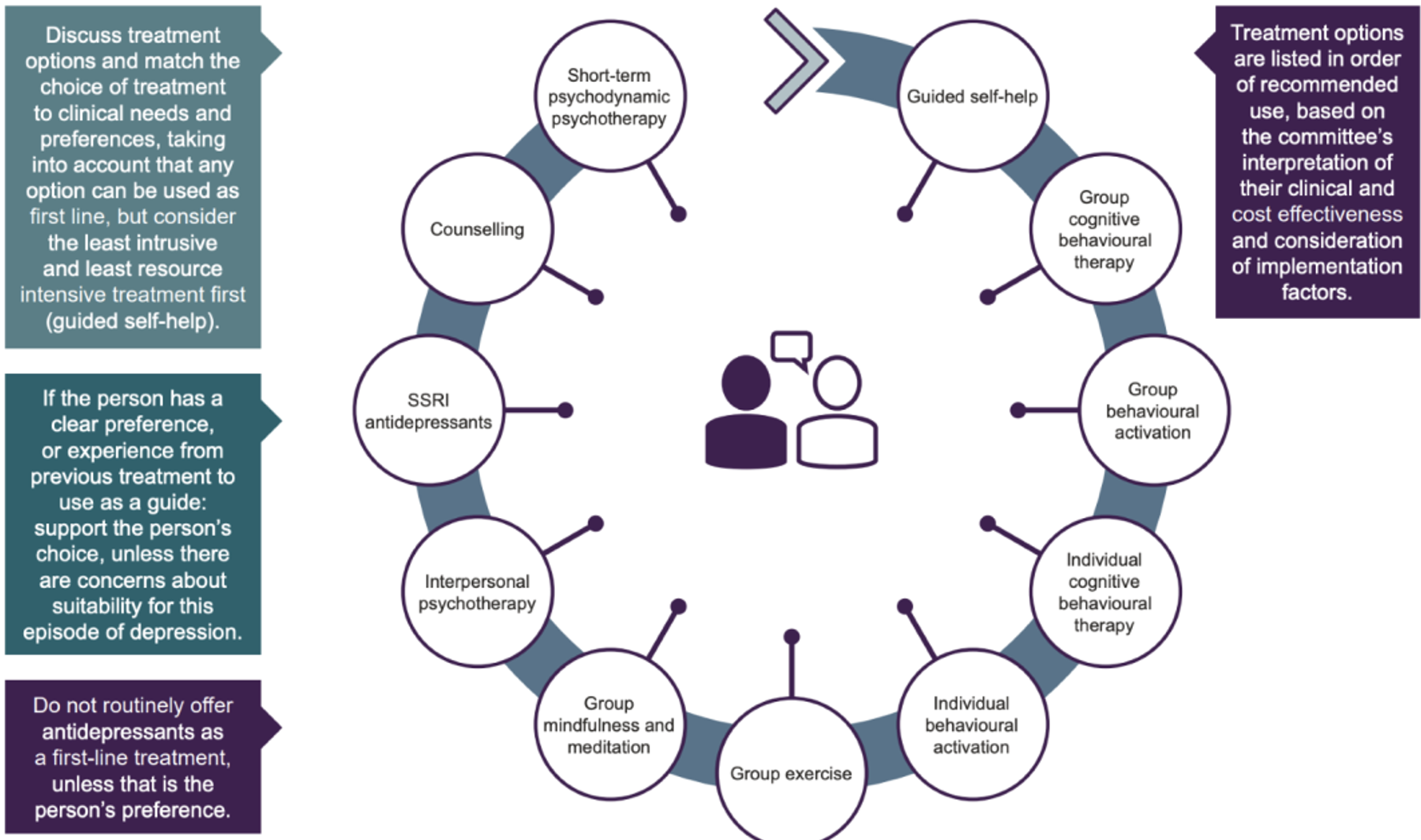
There are several ways to treat depression, usually combining psychotherapy and medication to effectively reduce symptoms and improve quality of life.
Psychotherapy plays an important role in the treatment of depression. Cognitive Behavioral Therapy (CBT) is a common approach that helps patients identify and shift negative thought patterns and teaches them healthier ways of coping with stress and difficulties. In addition, psychological support and counselling help patients express their emotions, build a support system, and learn to cope with emotional distress.
Medication is usually considered in cases of major depression or when psychotherapy fails to relieve symptoms. Antidepressant medications can regulate chemicals in the brain to help improve mood and emotional stability. However, medications need to be supervised by a doctor, as they can have side effects and need to be adjusted. Consult your doctor for details.
In addition, a healthy lifestyle is crucial in treating depression. Regular exercise, a balanced diet and adequate sleep help maintain physical and mental health. People with depression should also reduce stress, learn relaxation techniques, and find a support system.
Treating depression is a lengthy process, and each patient's needs are different. But by combining psychotherapy, medication and a healthy lifestyle, most patients can gradually improve their symptoms and regain their quality of life. For seniors, seeking help early and working with a team of healthcare professionals is the first step in overcoming the challenges of depression.
In closing, I want to tell you that although geriatric depression may sound far-fetched and not well understood by the general public, it is important to take a more active role in the mental health of older adults to prevent the dreaded disease from coming to your family. Everyone ages at some point, and in this fast-paced information society, seniors should never be left behind!
Citation:
1. American Psychiatric Association. (2013).Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
2. 黑马原创文章. (2021, January 5).心理学案例分析:老年人是一大抑郁症群体,却最容易被忽视.Www.sohu.com. https://www.sohu.com/a/442529546_120 571013
3. Smith, J. A., & Johnson, R. B. (2019). Genetic factors and depressive disorders in older adults. Journal of Gerontology, 45(2), 123-136.
4. Brown, L. M., & Jones, C. D. (2018). Social isolation and depression in the elderly: A qualitative study. Aging and Mental Health, 28(5), 567-582.
5. Williams, P. T., & Davis, M. R. (2020). Cognitive distortions and depression in older adults. Psychology and Aging, 33(3), 321-335.
6. O'Connor, S. M., & Wilson, E. J. (2017). Sociocultural factors and elderly depression: A cross-cultural analysis. Journal of Aging Studies, 22(4), 421-435.
7. DSM-5 Criteria for Major Depressive Disorder. (n.d.). https://www.mdcalc.com/calc/10195/dsm-5-criteria-major-depressive-disorder